1. What is Mental Health?
- Mental health refers to emotional, psychological, and social well-being.
- It influences how people think, feel, and act.
- It determines how we handle stress, relate to others, and make choices.
- Mental health disorders include depression, anxiety, bipolar disorder, PTSD, schizophrenia, etc.
2. How Big is the Problem? Global Data & Trends
Here are recent data points, showing scope, trends, and scale:
| Metric | Recent Figure / Trend | Source / Notes |
|---|---|---|
| Number of people with mental health disorders globally | Over 1 billion | WHO: more than 1 billion people live with a mental health condition such as anxiety or depression. (World Health Organization) |
| Leading causes of long-term disability | Mental health disorders are among the top reasons globally | Anxiety & depression especially common. (World Health Organization) |
| Economic cost | USD ~ 1 trillion per year (depression & anxiety alone) | Indirect costs (lost productivity), healthcare cost burdens. (World Health Organization) |
| Health-budget allocation | Median government spending on mental health ≈ 2% of total health budgets globally | Unchanged since 2017. (World Health Organization) |
| Mental health workforce density | Median ~ 13 mental health workers per 100,000 people | Low in low-/middle-income countries. (World Health Organization) |
| Increase since 1990 | Incidence rates rising (~15 %) between 1990-2021 | Global Burden of Disease study. (BioMed Central) |
Key Trend: COVID-19 Effects
- Depression and anxiety rates rose significantly during the pandemic. (Healthdata)
- Disruption of mental health services in many countries. (World Health Organization)
3. Risk Factors & Causes
Mental health disorders have multiple interacting causes:
- Biological: genetics, neurochemistry, brain injury.
- Psychological: childhood trauma, stress, adverse childhood experiences.
- Social & environmental: poverty, inequality, social isolation, conflict, disasters.
- Lifestyle: substance use, lack of sleep, poor diet, minimal physical activity.
- Cultural / societal stressors: stigma, discrimination, cultural transition.
4. Impact: Individuals, Society & Economy
Individuals
- Reduced quality of life.
- Physical health deterioration.
- Higher mortality (including from suicide).
Society
- Burden on health systems.
- Strain on caregivers and families.
- Social exclusion, increased crime, homelessness in some settings.
Economy
- Healthcare costs.
- Loss of productivity.
- Social welfare and support costs.
5. Treatment, Prevention & Support Systems
| Area | Key Components | Examples / Notes |
|---|---|---|
| Clinical Treatment | Therapy (CBT, counselling), medication, inpatient care | Need for access to psychiatrists, antidepressants, etc. |
| Prevention | Early detection, education, lifestyle interventions | School programmes, public awareness campaigns |
| Community / Peer Support | Support groups, peer counselling, helplines | Often more accessible, less costly |
| Digital & Telehealth Solutions | Apps, tele-counseling, remote therapy | Rapid growth, especially in settings with few professionals |
| Policy & Legislative Support | Mental health policy, rights-based laws, universal health coverage | Ensuring services are available, affordable, non-discriminatory |
6. Global Comparisons
Comparison by region, income level, prevalence, treatment gaps:
| Region / Country Type | Prevalence Rates / Key Metrics | Treatment Gap / Access | Notes |
|---|---|---|---|
| High-income countries | Higher “diagnosed” rates; more resources; higher reporting of depression & anxiety; higher ASIR (age-standardized incidence rate) in some regions. (BioMed Central) | Better access to mental health workers, services, insurance | But still stigma and unmet need persist. |
| Low- & Middle-Income Countries (LMICs) | Rising incidence; often under-diagnosed. (BioMed Central) | Severe shortage of mental health professionals; low budget allocations; high treatment gaps | E.g., many people don’t receive any treatment. |
| By Country Example: China | Large population; increasing focus on mental health: schools to have mental health edu, hospital availability targets. (Reuters) | Still gaps in rural areas; some mental health services recently scaled up. | |
| By Gender / Age | Women tend to show higher prevalence of anxiety / depression; adolescents & youth majorly impacted. (World Health Organization) | Youth often have special barriers: stigma, awareness, access |
7. Notable Government Initiatives Worldwide
Governments globally have launched programs, policies, laws to address mental health. Here are examples:
| Country / Region | Initiative | Key Features & Impacts |
|---|---|---|
| India | National Tele Mental Health Programme (Tele-MANAS) | 24×7 helpline (14416) in ~20 languages; thousands of calls; Tele-MANAS Cells established; digital solutions. (Mookerjee Foundation) |
| India | Jeevani Mental Health Program (Kerala) | College student focus; counselling in colleges; reaching tens of thousands. (Wikipedia) |
| China | Mental Health Service Expansion (2025-27) | Mental health hotlines; outpatient services for disorders; mental health education in schools. (Reuters) |
| California (USA) | Mental Health Services Act (MHSA) | Dedicated funding; community-based services; preventive & transformative programs. (Wikipedia) |
| USA | Safe Schools/Healthy Students grants | Partnership among education, health, justice sectors to make schools safer and provide mental health services. (Wikipedia) |
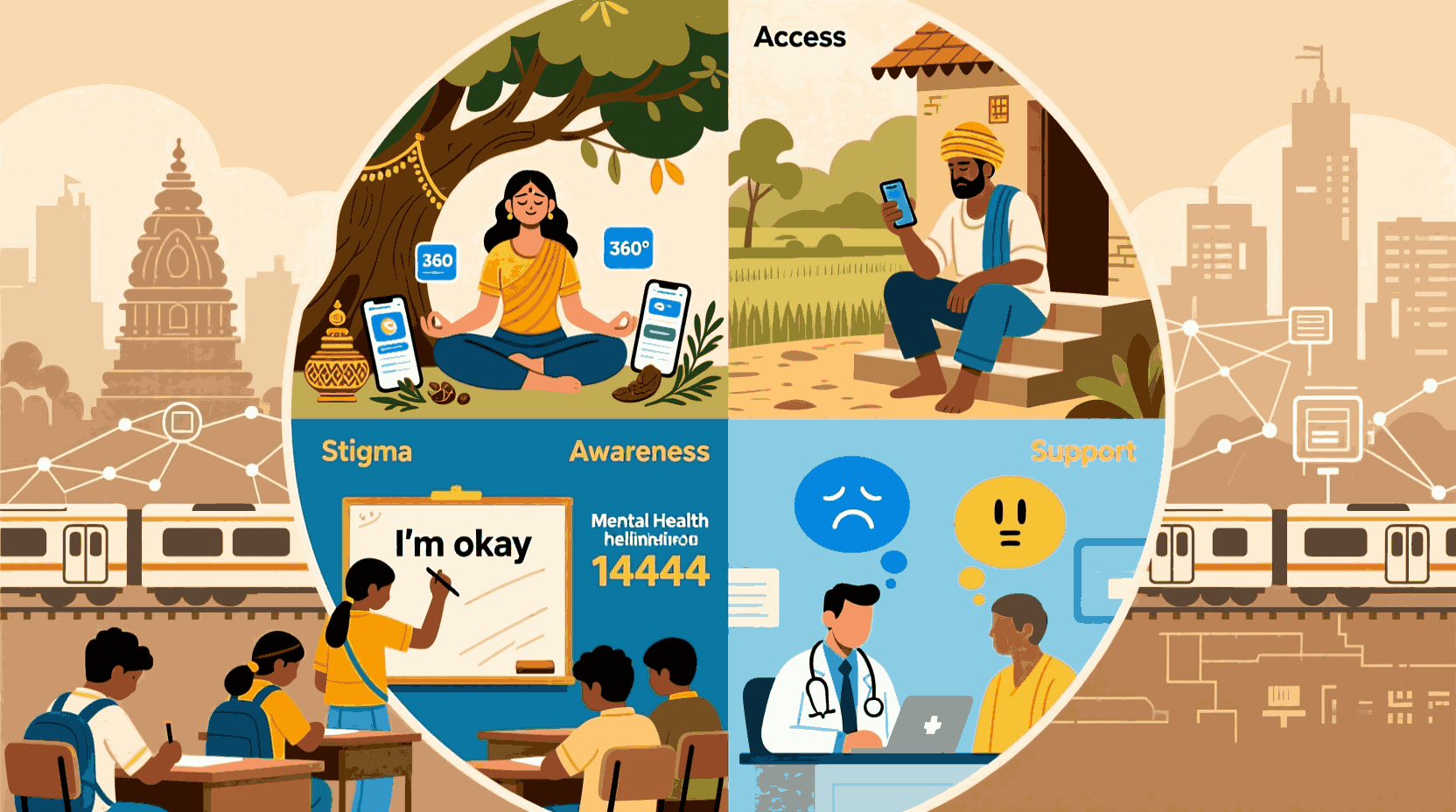
8. Challenges & Gaps
- Treatment Gap: Many with mental disorders get no treatment.
- Human Resources: Shortage of psychologists, psychiatrists, social workers.
- Funding: Mental health often underfunded; 2% of health budgets globally on average. (World Health Organization)
- Stigma & Cultural Barriers: Fear, discrimination, shame prevent help-seeking.
- Access & Inequality: Rural, low-income, marginalized populations less served.
- Quality & Continuity: Even where services exist, quality varies; continuity of care is weak.
- Legislation & Policy: Not all countries have mental health laws compliant with human rights. Enforcement weak. (World Health Organization)
9. Strategies for Improvement
To make real progress, multiple approaches are needed:
- Scaling up mental health services in primary care, integrating mental health into general health systems.
- Training & task-shifting: Use of non-specialist workers, peer counsellors.
- Digital interventions: Telehealth, apps, AI, remote therapy.
- Public awareness & anti-stigma campaigns.
- Youth & school programmes: Mental health education early on.
- Laws & policies: Rights-based mental health legislation, funding commitments.
- Cross-sector collaboration: Health, education, social welfare, justice, employment.
- Monitoring, data & research: Good data to drive policy; tracking outcomes; burden metrics.
10. Stigma, Awareness & Cultural Dimensions
- Stigma remains one of the biggest barriers. People fear being judged, losing jobs, social isolation.
- Culture shapes how mental health is seen – in some settings, mental illness is heavily stigmatized or attributed to supernatural causes.
- Language matters: how disorders are framed influences willingness to seek help.
- Community & peer support can help reduce stigma.
- Media, influencers, educational curriculum important in shaping awareness.
11. Future Directions & Emerging Trends
- AI & Digital Tools: Chatbots, online therapy, predictive analytics.
- Preventative mental health: focusing earlier in life; mindfulness; resilience training.
- Global policy momentum: WHO and UN SDGs emphasise mental health. (World Health Organization)
- Holistic approaches: Integrating mental, neurological, and substance use disorders; integrating social determinants.
- More inclusion of lived experience: service users shaping interventions & policy.
- Climate & environment as emerging stressors: displacement, disasters, eco-anxiety.
12. FAQ
Q1. How common are mental disorders globally?
Very common. Over 1 billion people live with mental health conditions. Anxiety and depression are among the most frequent disorders. (World Health Organization)
Q2. Do all countries have mental health laws?
Many do, but fewer have laws fully compliant with human rights standards. Enforcement and coverage vary. (World Health Organization)
Q3. How much do governments spend on mental health?
On average around 2% of health budgets globally. High-income countries spend much more per capita; low-income countries sometimes spend almost nothing. (World Health Organization)
Q4. What is the treatment gap?
A large fraction of people who need mental health services do not receive them. Barriers include access, cost, stigma, lack of providers.
Q5. Has mental health worsened after COVID-19?
Yes: prevalence of anxiety and depression increased; disruptions to service; indirect impacts like isolation, grief, economic stress. (Healthdata)
Q6. Which regions have the highest burden?
Low and middle income regions have large burdens, especially where resources are limited. But high-income regions also have high diagnosed rates. ASIR rising in low SDI regions. (BioMed Central)
Q7. What are cost-effective interventions?
- Integrating mental health in primary care.
- Task-sharing (non-specialist health workers).
- Psychosocial therapies.
- Digital/tele health.
Q8. What can individuals do?
- Seek help early.
- Use peer support, helplines.
- Adopt healthy lifestyle: sleep, exercise, nutrition.
- Learn stress management and mindfulness.
- Support others; reduce stigma.
Conclusion
Mental health is a major global challenge. Despite rising awareness, the data show that disorders like depression and anxiety remain under-treated. Governments and international bodies have initiated many promising programs, but gaps in funding, workforce, access, stigma, and policy persist. A holistic, multi-sector, and rights-based approach is essential. The good news: tools exist, lessons are being learned, and momentum is building. But much work remains.